When it comes to oral health, two terms often come up that might sound scary but are very important to understand: gingivitis and periodontitis. Both of these conditions affect the gums and can have serious consequences if left untreated. However, many people confuse the two or don’t know the significant differences between them. This article will walk you through everything you need to know about gingivitis vs. periodontitis in a clear, simple way so that you can take the best care of your smile.
Содержание
- 1 What is Gingivitis?
- 2 What is Periodontitis?
- 3 Main Differences Between Gingivitis and Periodontitis
- 4 How Are Gingivitis and Periodontitis Diagnosed?
- 5 Treatment Options: Tackling Gingivitis and Periodontitis
- 6 Preventing Gingivitis and Periodontitis
- 7 The Connection Between Gum Disease and Overall Health
- 8 Common Myths About Gingivitis and Periodontitis
- 9 Who is at Higher Risk for Gingivitis and Periodontitis?
- 10 The Role of Technology in Diagnosing and Treating Gum Disease
What is Gingivitis?
Gingivitis is the earliest stage of gum disease, characterized primarily by inflammation of the gums. It is the result of plaque buildup along the gumline, which contains bacteria irritating the gums. The symptoms of gingivitis include redness, swelling, and bleeding during brushing or flossing. The good news is that at this stage, the damage is reversible with proper dental care and good oral hygiene.
Most of us have probably experienced gingivitis without even realizing it. Since it doesn’t often cause pain, it can go unnoticed. Yet, it’s a warning sign that you need to improve your oral hygiene routine to avoid further problems.
Causes of Gingivitis
Gingivitis is primarily caused by plaque, a sticky film of bacteria that constantly forms on teeth and gums. If plaque is not removed regularly through brushing and flossing, it hardens into tartar, which can further irritate the gums. Other factors that can contribute to gingivitis include:
- Poor oral hygiene habits
- Smoking or tobacco use
- Hormonal changes during pregnancy or menstruation
- Certain medications such as steroids or chemotherapy drugs
- Conditions like diabetes that affect your immune system
- Stress or a weakened immune response
Symptoms to Watch For
Recognizing gingivitis early is key to stopping it before it progresses into a more severe condition. Here are the common symptoms you should keep an eye on:
| Symptom | Description |
|---|---|
| Red or Swollen Gums | Healthy gums are usually pink and firm. Inflamed gums appear red and swollen. |
| Bleeding Gums | Gums that bleed easily during brushing or flossing indicate irritation and inflammation. |
| Bad Breath | The bacteria in plaque can cause persistent bad breath or a bad taste in the mouth. |
| Tenderness | Gums may feel sore or tender to the touch, even if there is no pain when eating. |
What is Periodontitis?
Periodontitis is essentially the advanced stage of gum disease that occurs when gingivitis is left untreated. It is a serious infection that damages the gums and can destroy the bone that supports your teeth. Unlike gingivitis, periodontitis can lead to tooth loss and other complications if not addressed promptly.
The transition from gingivitis to periodontitis happens when harmful bacteria invade deeper into the gum tissues, creating pockets between the teeth and gums. These pockets become infected, and the body’s immune response causes the destruction of bone and connective tissue.
How Does Periodontitis Develop?
The progression from gingivitis to periodontitis is often gradual and silent. You might not notice much change in how your mouth feels initially. Over time, as the infection worsens, you might start to see more serious signs such as:
- Gum recession, where the gums pull away from the teeth
- Loose or shifting teeth
- Persistent bad breath despite good hygiene
- Formation of deep pockets between teeth and gums
- Pus between gums and teeth
Once periodontitis begins to damage the bone and tissues supporting teeth, it becomes more difficult to reverse the damage. Dental treatment is necessary to manage the disease and prevent tooth loss.
Symptoms of Periodontitis
Early symptoms might be similar to gingivitis but usually last longer and become more severe. Here’s a comparison table that highlights symptoms of both gingivitis and periodontitis:
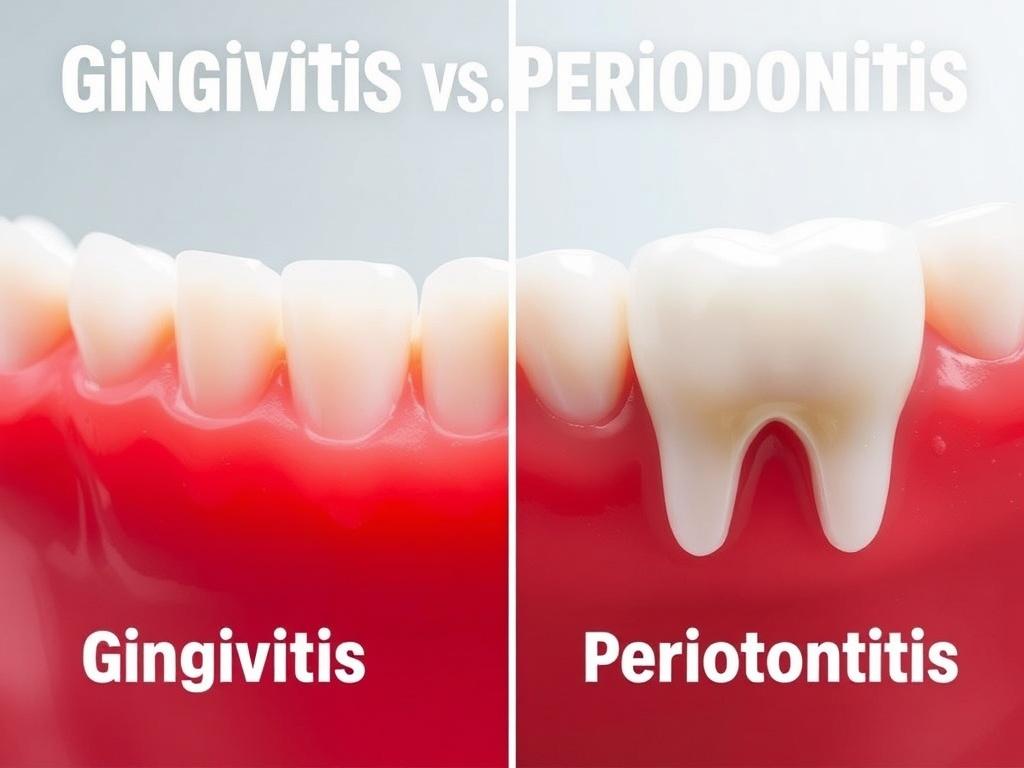
| Symptom | Gingivitis | Periodontitis |
|---|---|---|
| Gum Color | Red and swollen | Dark red or purple, swollen with possible recession |
| Bleeding Gums | Common during brushing/flossing | Frequent, with or without brushing |
| Bad Breath | Occasional | Persistent bad breath and bad taste |
| Pain | Rarely painful | May experience pain or discomfort |
| Tooth Mobility | No mobility | Teeth may become loose or shift |
| Pocket Formation | Absent or shallow pockets | Deep pockets between gums and teeth |
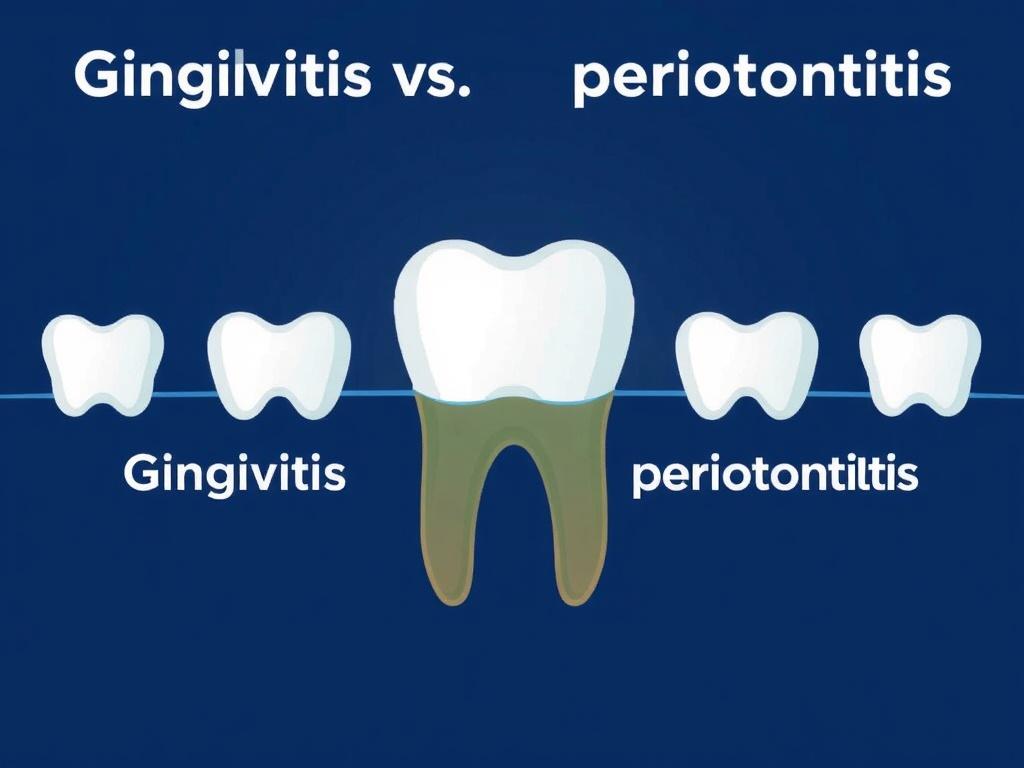
Main Differences Between Gingivitis and Periodontitis
Gingivitis vs. periodontitis can seem confusing because both involve gum inflammation, but the key differences lie in severity, reversibility, and impact on your oral structures. Here’s a simple breakdown:
| Aspect | Gingivitis | Periodontitis |
|---|---|---|
| Stage of Gum Disease | Early | Advanced |
| Reversibility | Fully reversible with good hygiene | Not fully reversible, requires professional treatment |
| Bone and Tissue Damage | No damage | Loss of bone and connective tissue |
| Treatment Needed | Improved brushing and flossing, professional cleaning | Deep cleaning, antibiotics, possibly surgery |
| Potential Consequences | Gingivitis may progress to periodontitis if untreated | Tooth loss, systemic health issues |
How Are Gingivitis and Periodontitis Diagnosed?
Dentists often spot gingivitis during routine dental exams by looking at the gums for swelling, redness, and bleeding. For periodontitis, they may perform additional tests, including measuring the depth of pockets around the teeth and taking x-rays to check for bone loss.
Routine dental visits are essential because you might not notice these conditions developing on your own. Early diagnosis means easier treatment and better outcomes.
Diagnostic Tools Explained
- Visual Examination: Checking for gum redness, swelling, and bleeding.
- Periodontal Probing: Using a small probe to measure the depth of gum pockets.
- X-rays: Reveal loss of bone supporting teeth.
- Medical History: Identifying risk factors such as smoking or diabetes.
Treatment Options: Tackling Gingivitis and Periodontitis
Treatment for gingivitis is straightforward and usually involves improving daily oral hygiene and receiving professional cleanings. However, treating periodontitis is more complex and might require several steps.
Treating Gingivitis
If you have gingivitis, your dentist or hygienist will perform a professional cleaning to remove plaque and tartar. They will also guide you on how to better brush and floss to keep bacteria at bay. Sometimes, an antimicrobial mouthwash may be recommended.
Treating Periodontitis
Treating periodontitis aims to control infection and prevent further damage. Common treatments include:
- Scaling and Root Planing: Deep cleaning below the gumline to remove plaque and tartar.
- Antibiotics: Topical or oral medications to fight infection.
- Surgery: In severe cases, surgical procedures like flap surgery or bone grafts may be necessary.
Staying consistent with professional dental care and personal oral hygiene is critical during and after treatment.
Preventing Gingivitis and Periodontitis
Prevention is always better than cure when it comes to gum diseases. Regular brushing, flossing, and dental checkups are your best defense. Here are some tips to keep your gums healthy:
- Brush twice daily using fluoride toothpaste.
- Floss daily to remove plaque between teeth.
- Visit your dentist every six months for cleanings and checkups.
- Avoid tobacco use.
- Eat a balanced diet rich in vitamins, especially vitamin C and calcium.
- Manage medical conditions like diabetes carefully.
The Connection Between Gum Disease and Overall Health
Did you know that gum disease can affect more than just your mouth? Research has shown links between periodontitis and systemic conditions such as heart disease, diabetes, and respiratory problems. The inflammation caused by gum disease may contribute to these health issues, making it even more important to maintain gum health.
Why Taking Gum Health Seriously Matters
When bacteria invade the gums, they don’t just stay there; they can enter your bloodstream and trigger inflammation throughout your body. Especially for people with pre-existing health concerns, untreated periodontitis can worsen outcomes or increase risks for complications.
Common Myths About Gingivitis and Periodontitis

Misunderstanding these conditions can prevent people from seeking care. Let’s clear the air on some myths:
- Myth: “Bleeding gums are normal and nothing to worry about.”
Fact: Bleeding gums are a sign of inflammation and should never be ignored. - Myth: “Only older people get periodontitis.”
Fact: Gum disease can affect anyone at any age if oral hygiene is poor. - Myth: “If my gums don’t hurt, my gums are healthy.”
Fact: Gum disease may not cause pain until advanced stages. - Myth: “Brushing harder will get rid of gum disease.”
Fact: Harsh brushing can worsen gum problems; gentle, effective brushing is best.
Who is at Higher Risk for Gingivitis and Periodontitis?
Some groups are more likely to develop gum disease, including:
- Smokers
- Pregnant women (due to hormonal changes)
- People with diabetes
- Individuals with poor oral hygiene habits
- Those under chronic stress
- People taking certain medications that reduce saliva flow
If you fall into any of these categories, it is especially important to be vigilant about your gum health.
The Role of Technology in Diagnosing and Treating Gum Disease
Modern dentistry has made great strides in managing gum disease thanks to advanced technology. Laser treatments, digital imaging, and improved surgical techniques offer more precise and effective care with less discomfort. Additionally, new diagnostic tools allow dentists to detect early-stage gum disease even before symptoms appear.
By combining these technologies with traditional oral care, dental professionals can better guide patients through treatment and prevention.
Conclusion
Understanding the difference between gingivitis vs. periodontitis is essential for maintaining healthy gums and a bright smile. While gingivitis is the early, reversible stage of gum disease characterized by inflammation and bleeding, periodontitis is a more serious and potentially irreversible condition that affects the bone and tissues supporting your teeth. Both are primarily caused by plaque buildup and can often develop silently without pain, underscoring the importance of regular dental checkups and good oral hygiene habits. By recognizing symptoms early, seeking timely dental care, and adopting preventive measures such as proper brushing, flossing, and lifestyle choices, you can protect yourself from the progression of gum disease and even preserve your overall health. Remember, healthy gums are not just about a beautiful smile—they are a vital part of your well-being.